February 2018
Questions and Answeres About Ovulation Induction
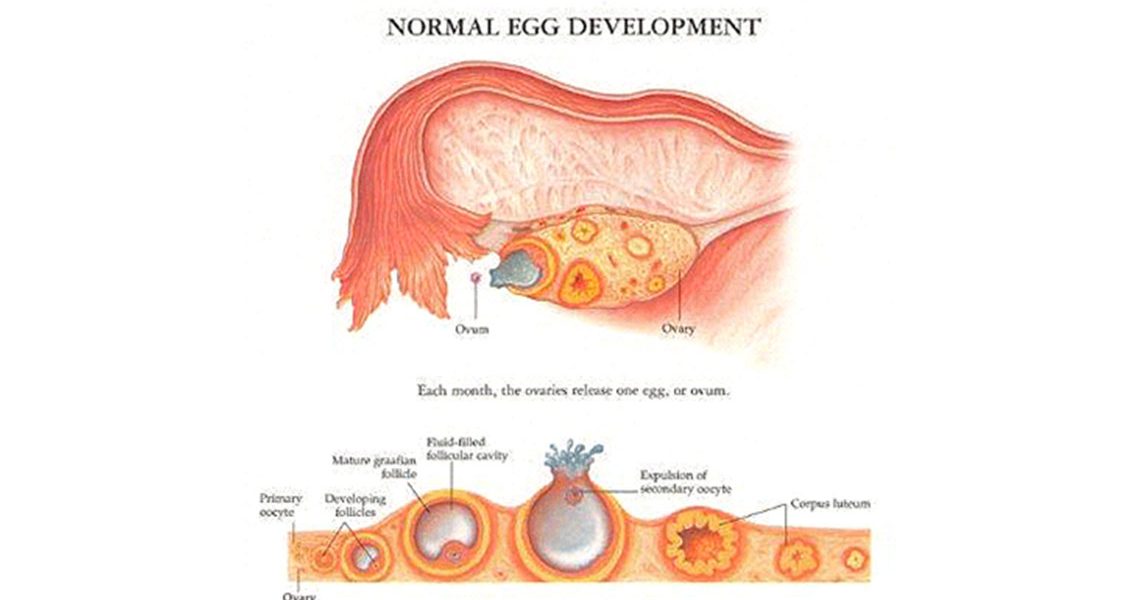
What is ovulation?
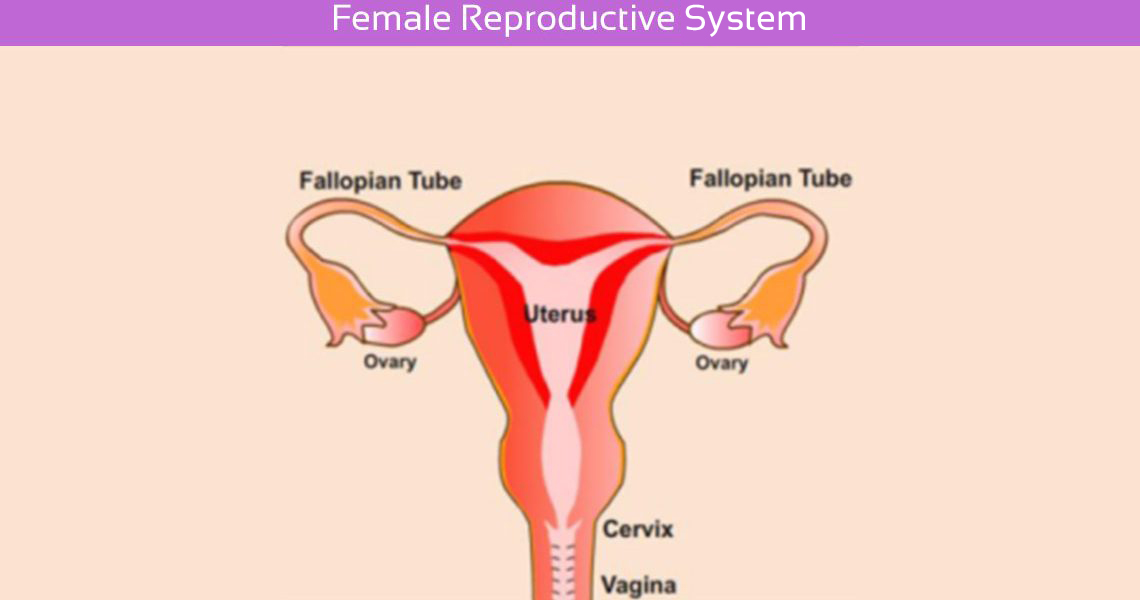
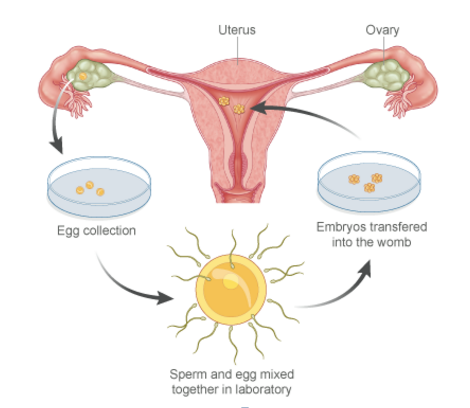
Usually each month one ovary will be stimulated by hormones produced in the brain. These cause a small cyst or follicle to grow on the ovary in which an egg develops. Another hormone then causes the follicle to release one egg to travel down the fallopian tube where it can be fertilized by the sperm which swims up from the vagina. This usually occurs around 14 days after the beginning of a period but can vary between 11 – 16 days.
Myths about Infertility
Myth 01: Infertility is rare.
Infertility can affect women of any age and from any background. In fact, approximately one out of every seven couples trying to conceive today experience difficulties with infertility. The Centers for Disease Control and Prevention (CDC) reports that 12 percent of women in the U.S. ages 15 to 44 have difficulty getting pregnant or carrying a pregnancy to term. That’s nearly one in five women in the U.S. So it’s likely that you know someone struggling with infertility, whether they choose to share it or not.
Impacts of Infertility on the couples Relationships?
Men and women are affected by infertility in different ways.
10 Early Signs of Pregnancy?
1. Prickling, tingling nipples
As pregnancy hormones increase the blood supply to your breasts, you may feel a tingling sensation around your nipples.
This can be one of the earliest symptoms of pregnancy and is sometimes noticeable within a week or so of conception. Once your body gets used to the hormone surge, this sensation will subside.