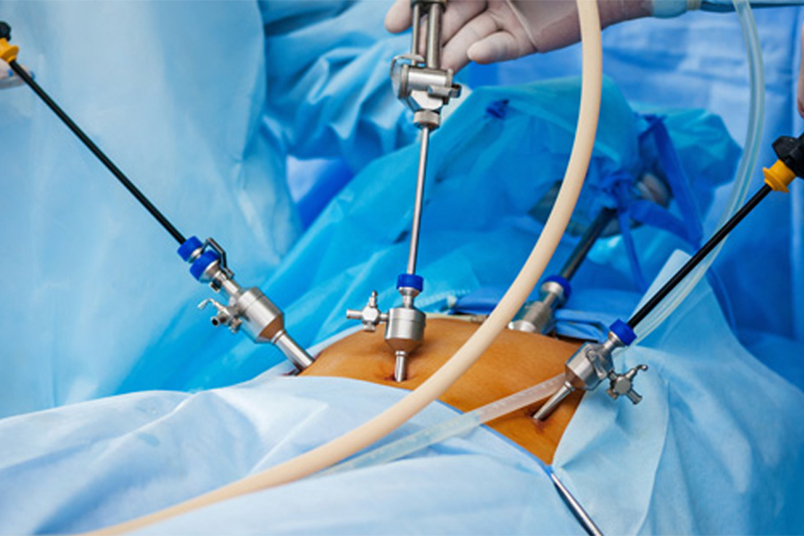
Dr. Abhilash E. is our esteemed Reproductive Medicine Specialist and Gynaec Laparoscopic Surgeon at NU Hospitals, Shivamogga. With a sincere commitment to helping individuals navigate their parenthood and fertility journeys,
Dr. Abhilash combines substantial expertise with genuine empathy to deliver personalised care. His strong educational background, including an MBBS, MS in Obstetrics & Gynaecology, and fellowships in Reproductive Medicine and advanced Laparoscopy, makes him a highly qualified professional in addressing a wide range of fertility challenges.
He has previously worked in a renowned IVF chain Hospital and has experience performing 2000+ IVF procedures and 500+ fertility-related laparoscopic procedures