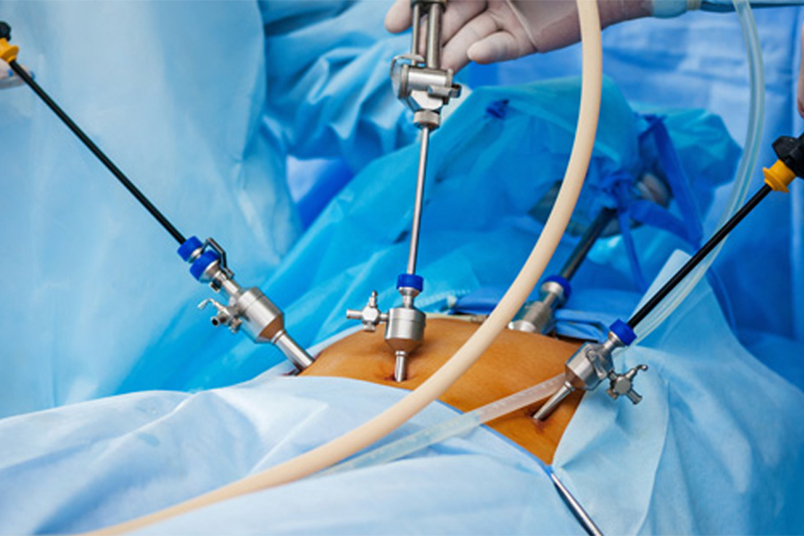
Laparoscopy, also known as minimally invasive surgery, is a common procedure used to diagnose and treat various conditions, including infertility. This procedure involves the insertion of a thin, lighted tube through small incisions in the abdomen, providing a detailed view of the reproductive organs.
In case of infertility, laparoscopy helps in identifying and addressing various abnormalities that may hinder conception. If you are scheduled for laparoscopic surgery to address infertility issues, understanding what to expect before, during, and after the procedure can help improve concerns and ensure a smoother experience.
Following are pregnancy-related medical conditions that affect infertility and how Laparoscopy helps in identifying and treating these conditions.
- Pelvic inflammatory disease (PID): Laparoscopy may be recommended to assess and treat pelvic inflammatory disease, which can result from infections such as chlamydia or gonorrhoea. PID can cause scarring and blockage of the fallopian tubes, hindering the passage of eggs and sperm.
- Endometriosis: Laparoscopy is commonly used to diagnose and treat endometriosis, a condition where tissue similar to the lining of the uterus grows outside the uterus. Endometriosis can lead to pelvic pain, inflammation, and fertility issues.
- Fallopian tube evaluation: Blocked or damaged fallopian tubes can prevent the egg from meeting the sperm, leading to infertility. Laparoscopy can help visualize the tubes and address any blockages or abnormalities.
- Ovarian cysts: Laparoscopy may be used to remove ovarian cysts or determine their impact on fertility. Large cysts or those affecting normal ovarian function can interfere with ovulation and conception.
- Uterine abnormalities: Laparoscopy can be employed to evaluate the structure of the uterus for abnormalities such as uterine fibroids, polyps, or congenital malformations that may affect fertility.
- Adhesions and scarring: Previous surgeries or infections can lead to the formation of adhesions and scarring within the pelvic cavity, affecting the normal functioning of reproductive organs. Laparoscopy can identify and, in some cases, address these adhesions.
- Unexplained infertility: In cases where the cause of infertility is not clear, laparoscopy may be performed to visually inspect the pelvic organs and identify any subtle abnormalities that may not be evident through other diagnostic methods.
- Ovulatory disorders: Laparoscopy may be considered when there are concerns about ovulatory disorders, such as polycystic ovary syndrome (PCOS), and other conditions affecting the ovaries.
Preparing for the Laparoscopy
A] Preoperative guidelines
Before the surgery, your healthcare provider will provide specific guidelines to ensure optimal preparation. These may include:
Stage 1· Medical evaluation: You will undergo a thorough medical evaluation to assess your overall health. This may involve blood tests, imaging studies, and a detailed discussion about your medical history.
Stage 2· Fasting: Typically, you will be asked to refrain from eating or drinking for a certain period before the surgery. This is to minimize the risk of complications during anaesthesia.
Stage 3· Medication review: Inform your healthcare provider about any medications or supplements you are taking. Some may need to be temporarily discontinued, while others can be taken with a sip of water.
Stage 4· Consent and discussions: Your surgeon will explain the procedure, potential risks, and benefits. It is essential to ask questions and address any concerns, ensuring informed consent.
B] Day of the Surgery
Stage 5· Admission process: On the day of the surgery, you’ll be admitted to the hospital or surgical centre. The nursing staff will guide you through the admission process, checking vital signs and confirming details.
Stage 6· Anaesthesia: Before the procedure, you’ll be administered anaesthesia, which may be general or regional depending on the complexity of the surgery. The anaesthesiologist will discuss this with you before the surgery.
Stage 7· Surgical procedure: Once under anaesthesia, small incisions will be made, and the laparoscope will be inserted. The surgeon will explore the pelvic area, identify any abnormalities, and perform necessary interventions such as removing cysts or treating endometriosis.
C] Recovery and Postoperative Care
Stage 8· Immediate post-op: After the surgery, you’ll be taken to the recovery room where the healthcare team will monitor your vital signs as you wake up from anaesthesia. Mild pain and nausea are normal initially.
Stage 9· Hospital stay: Depending on the complexity of the procedure, you may need to stay in the hospital for a day or go home on the same day. Your surgeon will provide specific postoperative care instructions, including wound care, activity restrictions, and prescribed medications.
Stage 10· Pain management: It is common to experience mild to moderate discomfort after laparoscopic surgery. Your healthcare provider will prescribe pain medications and recommend strategies to manage pain at home, such as rest and applying hot compression.
D] Recovery at Home: Taking Care of Yourself
Stage 11· Rest and activity: Adequate rest is crucial for healing. While rest is essential, gentle movement and walking are encouraged to prevent complications like blood clots. However, avoid strenuous activities during the initial recovery period.
Stage 12· Follow-up appointments: Follow-up sessions help your surgeon monitor your recovery and ensure that your body is healing properly. This is also the time for you to ask and discuss any concerns or questions you may have with your gynaecologist.
Stage 13· Emotional support: Dealing with infertility and undergoing surgery can be emotionally challenging. Seek support from friends, family, or counselling services to navigate these feelings effectively.
References:
- IVF. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK562266/.
- Preparing for IVF. Society of Assisted Reproductive Technology. https://www.sart.org/patients/a-patients-guide-to-assisted-reproductive-technology/general-information/preparing-for-ivf-emotional-considerations/.
- IVF. Create Fertility. https://www.createfertility.co.uk/blog/10-things-you-should-know-about-ivf.
- IVF. Human Fertilization & Embryology Authority. https://www.hfea.gov.uk/treatments/explore-all-treatments/in-vitro-fertilisation-ivf/.