What is low testosterone?
Testosterone is an important hormone for men. Produced by the testes, the hormone gives men many of their masculine characteristics, like facial hair and a deeper voice. It is involved with sperm production and sex drive. It also contributes to strength, bones, and muscle mass.
Low testosterone, also called hypogonadism, occurs when a man’s body doesn’t produce adequate amounts of the hormone.
Hypogonadism can happen if there is a problem with the hypothalamus or pituitary gland (two areas of the brain that help trigger the production of testosterone) or with the testes themselves. For example, men who have both testes removed during treatment for testicular cancer would no longer produce enough testosterone.
What is Andropause?
The normal course of aging can also cause men’s testosterone levels to decline. This process is sometimes called “andropause,” as a comparison to female menopause. However, the drop in testosterone is much more gradual for men than the drop in estrogen that women experience. Generally, men’s testosterone levels start to decrease by about 1% each year around age 30.
The Urology Care Foundation estimates that 4 out of 10 men over age 45 have low testosterone levels.
Low testosterone has also been linked to diabetes, high blood pressure, high cholesterol, obesity, HIV infection, AIDS, and long-term opioid use.
What are the symptoms?
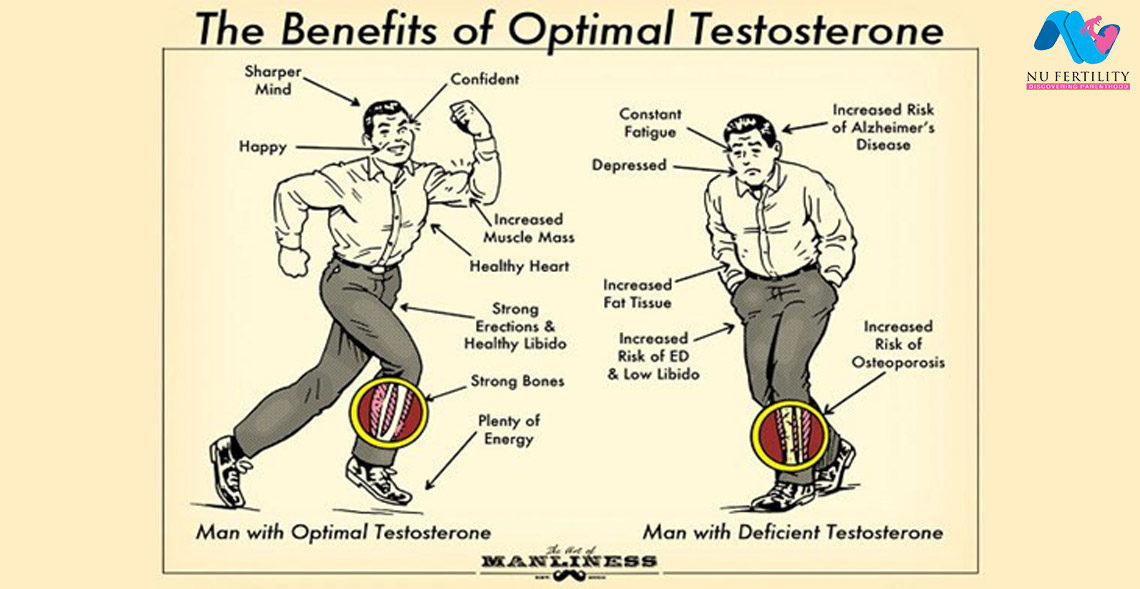
Common symptoms of low testosterone include the following:
- Reduced sex drive, less interest in sex
- Erectile dysfunction (weaker erections or trouble getting an erection)
- Decreased muscle mass
- Mood swings and/or depressed mood
- Fatigue
- Enlarged male breasts
- Anemia
- Loss of calcium from bones
How is it diagnosed?
Low testosterone is diagnosed with a blood test. A man’s testosterone levels fluctuate throughout the day, but they are usually highest in the morning. Many doctors prefer to test at that time (7am-10am). In general, a man is diagnosed with low testosterone if his level is below 300 ng/dL.
Sometimes, a distinction is made between bound, free, and total testosterone. About 98% of testosterone in the body is bound. This means it is attached to proteins – albumin and sex hormone binding globulin (SHBG) – that help it travel through the bloodstream. The rest is considered free. It is not attached to any proteins. Usually, free testosterone is the type connected with sexual problems.
Most of the time, doctors check total testosterone, the combination of bound and free taken together. This measurement is used to diagnose hypogonadism.
A doctor might also check levels of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) since these hormones work with the testes.
How is low testosterone treated – Testosterone therapy:
Many men diagnosed with hypogonadism find that testosterone therapy helps recover their sex drive and improve their mood. However, it may not help with erectile function if there are underlying causes of that condition, such as diabetes or heart disease.
Testosterone therapy can be administered in several ways:
- Gels: Most men choose this option. A testosterone gel is applied to the skin daily, usually on the upper arm or shoulder. Men using a gel should wash their hands thoroughly after applying it. They should also be careful to cover the area and make sure that the gel does not rub off on another person’s skin.

Testosterone gel application
- Patches: Testosterone patches stick to the skin on a man’s upper arm, back, stomach, or thigh. Used daily, patches should be rotated to different areas so that the same spot isn’t used more than once every seven days.
- Injections: Testosterone shots can be administered by a doctor or by the man himself. They are usually needed every one to three weeks, though longer-acting preparations may be used every 3 months.
Depending on the treatment method, testosterone levels may remain constant throughout the day or they may rise in the morning and decrease in the evening, as is typical in the body.
A man’s doctor can help him decide which method is best for him.
Men should not take testosterone if their levels are normal or if they haven’t been tested. The diagnosis of low testosterone should always be made by a qualified healthcare provider.
Follow-up?
Following up with an Andrologist/Urologist is important for men on testosterone therapy. Generally, these men should have their testosterone levels checked every 3-4 months during the first year. This can be done with a simple blood test.
The best time of day for the blood test depends on the type of therapy being used. For men using a patch, testosterone levels tend to be highest about four to eight hours after application. However, men using gels can usually have their levels checked at any time since this delivery system tends to keep levels constant throughout the day.
It’s also recommended that men on testosterone therapy periodically have digital rectal exams and PSA (prostate-specific antigen) tests to keep an eye on their prostate health.
Because testosterone therapy can increase red blood cell counts, men should also have their hemoglobin levels checked regularly.
Side effects of Testosterone therapy:
Like any treatment, testosterone can have risks and side effects.
Some of the more common side effects of testosterone therapy include the following:
- Itching and irritation. This may occur wherever a testosterone patch or gel is applied. It tends to be less common for gel users.
- Increase in body hair
- Hot flashes
- Changes in cholesterol levels
- Changes in red blood cell counts
- Weight gain- due to salt and water retention (not fat accumulation)
- Acne and/or oily skin. This side effect usually ends when a man stops taking testosterone.
Testosterone therapy also lowers sperm counts, so it is generally not recommended for men with fertility concerns.
Although no conclusive evidence exists, testosterone therapy is suspected to spur the growth of prostate cells and prostate cancer cells. Men with prostate cancer are usually advised against testosterone therapy. Men should be screened for prostate cancer before starting treatment.
To avoid transferring testosterone to another person, men using the gel should wash their hands immediately after applying it. Before sex, they should shower or cover the application site so the gel doesn’t transfer to the partner. For example, since men usually apply the gel to the shoulders, upper arms, or abdomen, some men wear a shirt during sex.
Reluctance to discuss sexual problems?
Some men are reluctant to discuss their symptoms with a doctor, especially if they are having trouble performing sexually. In some cases, men buy over-the-counter testosterone products online or in stores. But this practice is risky, as some products contain other ingredients that can interact with drugs a man is already taking. It is always safer to see an Andrologist/Urologist.
In spite of the difficulty of discussing sexual symptoms with a doctor or a sex therapist, men who overcome their embarrassment find that receiving proper professional information and sexual counseling may contribute to successful medical treatment by testosterone.